From transplantation to bioengineering, the future of reproductive technology solutions offers hope for those facing infertility
When Kayla Edwards turned 13, she began to wonder if she was different. It started as a seed of suspicion when her friends began their menstrual cycles, and hers never arrived. Her grandmother was late, she learned, but for Edwards, it still seemed odd. She had hit puberty’s other benchmarks—the hormones, the breasts—just no cycle.
At 15, still absent a period, it was clear something was wrong, so her mother brought her to the obstetrician. During the examination, all her bloodwork came back normal, but, strangely, the doctor couldn’t locate her cervix. She ordered an ultrasound and a full-body CT scan, then finally, after a long wait returned, mystified. “I have never seen this before,” Edwards’ doctor admitted. “You have completely normal ovaries, but you’re missing your cervix and uterus,” she said, “I’m sorry to tell you that you will never be able to carry your own children.”
For the rest of her teenage life, Edwards told no one about her condition. “I felt so alone, so broken,” she said, “I didn’t feel like a woman.” But it wasn’t until years later, after Edwards fell in love and got married, that the gravity of her condition truly hit home.
She and her husband desperately wanted children—their own children—but Edward’s condition rendered that impossible. One night, she and her husband sat down to watch their favorite show, Survivor. One of the contestants, Jaclyn Schultz, started talking about why she came on the show. She wanted to raise awareness about a condition she was born with known as Mayer–Rokitansky–Küster–Hauser (MRKH) Syndrome, a congenital abnormality that affects nearly 1 in 5000 women worldwide. It’s a condition that stunts the development of the reproductive tract in utero, causing an under- or completely undeveloped uterus, cervix, or vaginal canal. Because of it, Schultz, like Edwards, was wombless since birth. “I literally jumped out of bed,” said Edwards. For the first time in her life, Edwards found someone like her, and for the first time, her condition had a name.
MRKH is just one of a number of devastating conditions that prevent a woman from bearing her own children. Other women may be forced to have a hysterectomy after cancer, or pregnancy trauma can make subsequent childbearing impossible. Whatever the cause, as many as 1 in 500 women worldwide are infertile due to uterine factors, a source of great pain and emotional anguish to many. For all these women, there have been no remedies, save adoption or surrogacy—but that has all changed in recent years.

Due to pioneering advances in fields like transplantation and bioengineering, women like Edwards are now able to carry their own children. Edwards, in fact, has now given birth to her own child thanks to a new procedure that may well be the first of many to offer new hope to infertile women [3].
Uterus transplantation
In 2008, Swedish gynecologist Liza Johanneson was in the midst of her residency at the University of Gothenburg, Gothenburg, Sweden, when she came across her first MRKH patients (Figure 1). Their stories were devastating—the shame and loneliness they experienced as teenagers. Some would even carry tampons around in their bags to feel normal. Eventually, like Edwards, they grew desperate for children of their own.
Johanneson began to wonder if something could be done. In the early 2000s, surgeons in Saudi Arabia had completed the first uterus transplant, but it didn’t last long enough in the patient’s body to complete a pregnancy [4]. A professor at Gothenburg caught wind of her interest, and asked if she had any interest in working with him on uterus transplantation in rats, which would earn her a Ph.D. in return. “I sincerely thought he was crazy at first,” she said, but her experience with infertile patients, and their desperation to carry children, eventually led her to say yes.
The first few years of the study flew by. The rat study was overwhelmingly successful, with multiple successful deliveries of normal pups [1]. They began transplants in larger animals, and ultimately to nonhuman primates, baboons, and cynomolgus macaques [2].
After these successful trials, they applied for ethical permission to conduct clinical trials in women with uterine infertility, and by 2012, the year Johanneson defended her thesis, six of the nine women they had transplanted with uteri from living donors delivered healthy babies, the first human babies born from transplanted uteri in the world. “I’ve been very fortunate because it’s very rare for a physician or a researcher or scientist to start something and then see that idea through the whole way,” she said (Figure 2).
Uterus transplantation centers quickly began opening around the world, including one in Dallas at the Baylor University Medical Center, which recruited Johanneson as the medical director of uterus transplant in 2016. Edwards was one of Johanneson’s first patients, and after a few false starts, she gave birth to a baby girl. “She’s just the best thing that’s ever happened to me and my husband,” said Edwards, “we often just stare at each other like, ‘Oh my gosh, look what we did!’ I can’t believe what we were willing to go through to get her.”
Trouble with transplants
Edwards had a remarkably easy pregnancy, but getting pregnant was anything but simple. To even be considered for a transplant, she and her husband had to quit their jobs and move to Dallas from Washington State—that was in 2016. Then, their first donor fell through. Three months went by, then six and still, no match. Eventually, they found another donor, but Edwards had too many antibodies then, so she would have rejected the transplant. Finally, in 2017, they found a donor—a nurse from the very same hospital who had already had her kids, and no longer had a use for her uterus. “The uterus is actually a perfect organ to give away,” said Johanneson. Unlike a kidney or liver, which a live donor may need later in life, “if you’re done with your childbearing years, you really don’t need your uterus anymore,” she said.

After her surgery, Edwards had a tough recovery. She remained in the intensive care unit (ICU) for a few days, in tremendous pain. Immunosuppressant drugs made her constantly weak and tired. It took a full month for her to feel normal again but then, finally, she had her first menstrual period, at the age of 24.
Before surgery, Edwards had already gone through in vitro fertilization (IVF) treatment to harvest eggs, and after the surgery, she went on IVF hormones to ready her body for pregnancy. The first embryo didn’t produce a pregnancy, nor did the second; still post-surgery, she had to go through a second IVF cycle for more eggs. The couple hadn’t had to pay for the transplant because it was a trial, but they did have to pay for IVF, at US$15,000 a cycle. They were beginning to fear they would run out of money and the entire effort would be for nothing, when finally, a full year after the transplant, the second embryo took. Edwards was pregnant.
(Photo courtesy of WFIRM.)
On September 19, 2019, after 36 weeks and two days in utero, Indy Pearl was born. Because she was a little early, she was born with jaundice, a common condition in preterm babies, so she spent a few days in the neonatal intensive care unit (NICU) before being released to Edwards and her husband. The pregnancy would be Edwards’ last. Though some women are able to keep their transplanted uterus and give birth to subsequent children, Edwards had developed gestational diabetes during pregnancy, which damaged her kidneys, so her doctors ordered she have a hysterectomy. And just like that, Edwards lost the uterus she had worked so hard to acquire.
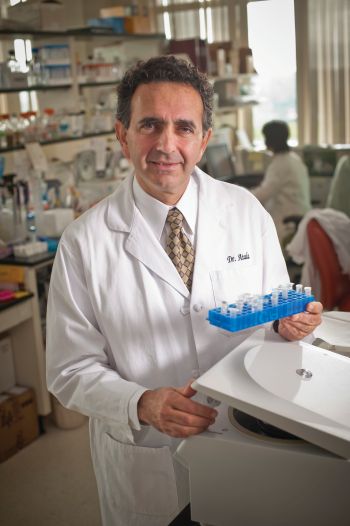
Such is a common drama with transplants. Transplantation “is a great option, but you are then dealing with issues from antirejection medications, as well as rejection of the organ itself,” said Anthony Atala, a pediatric surgeon and the director of the Wake Forest Institute for Genomic Medicine, Winston Salem, NC (Figure 3). And beyond that, he said, transplantation also leads to an increased risk of tumor formation. But right now, transplantation is the only solution for women like Edwards. “Having engineered tissue that can be used to correct these abnormalities is a medical need,” said Atala.
Bioengineered womb
As was the case with Edwards, a patient’s journey through the transplantation process is inevitably a saga. It takes a long time to find a donor with a blood type that matches the recipient’s, and even then, there are no guarantees the patient’s body will accept the foreign organ. But an organ engineered from the patient’s own tissue would cut out the need for both a donor, and the risk of rejection. The transplantation conundrum is what ultimately inspired Atala to wonder if there might be another option for these women. In 1999, Atala and his colleagues famously grew the first whole organs in a lab—bladders—which were transplanted in young patients with severe spina bifida [5]. They extracted cells from the children’s malfunctioning bladders and used them to grow thin sacs of tissue in the laboratory, creating rudimentary organs that were then grafted back on to the patients’ own, existing bladders.
In 2002, the year he published his successful results on the bladder transplant, Atala turned his attention to exploring whether the same idea might work for a uterus. But quickly he found that it was not going to be so simple—the uterus is just a much more complex organ. It has to support embryo implantation and fetal development, and that means you can’t just take a piece of tissue, place it into an existing organ, and expect it to grow and function. The tissue has to respond to the expansion and mechanical strains that occur during pregnancy. To engineer a lab-grown uterus with any hope of working, Atala and his team explored a technique—3D scaffolding to support, and shape, new cell and tissue growth. “We had to really work very hard to make sure that we had the cell biology down,” as well as the physiology, pharmacology, and biochemistry, he said, and only then could they think about actually growing the cells on the scaffolding. The work also had to be done in such a way that flexible tissues capable of supporting a pregnancy would grow. The uterus is made up of three major layers of tissue—the myometrium (a muscle), the submucosa, and endometrium—and all three were needed. Atala began experimenting with layering the cells. “We put the muscle cells on one side, we put the endometrial cells on the other side, and so we were creating, and really guiding, this layered structure in the same manner that the normal tissue would grow,” he said.
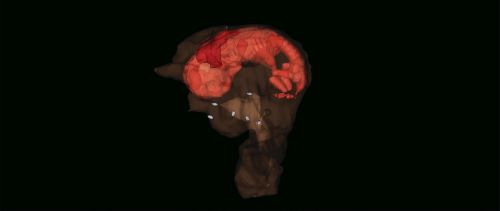
In the spring of 2020, in Nature Biotechnology, Atala and his colleagues announced a monumental success. They had grown a fully tissue-engineered rabbit uteri capable of carrying live young to term (Figure 4) [5]. They did it using a biodegradable polymer mesh scaffolding, upon which they placed cells, one at a time, to eventually grow layers of the rabbit’s own cells. In 78 rabbits, they then replaced each rabbit’s uterus with either a mesh structure containing seed cells, a mesh structure without seed cells, or they simply sutured the area with the missing organ. Six months later, the rabbits with the cell-seeded scaffolding developed a tissue structure resembling a uterus. Around this time, they mated 42 of the rabbits naturally, and ten of those with transplanted bioengineered uteri became pregnant. Of those, four completed normal pregnancies, giving birth to completely normal pups [6].

or tissue engineering, “this is a major achievement in the field,” said Robert Lanza, a pioneering stem cell researcher and head of Global Regenerative Medicine at the Astellas Pharma (Figure 5), but it’s just the beginning. “It really represents us moving into more complex organs with higher functional requirements,” he said. Ultimately, the “holy grail,” he said, is to engineer an entire kidney, but other reproductive systems may come first, including the cervix and fallopian tubes. “We’re in an exciting time where we’re finally getting the knowledge and skillsets to actually go for these more complex tissues,” he said.

(Photo courtesy of Ellie Nisbet Photography.)
But for now, there is still much work to be done. Atala needs to continue perfecting the procedure before working with human models. “We’ve spent 18 years getting to this point,” he said, “but we need to keep working because the paramount goals are really safety and efficacy, and we want to make sure that’s the case before we put anything into a patient.”
Life after transplant
Edwards, her husband, and their now 18-month daughter have moved back to Washington State. They’re looking to buy a house, and Edwards is trying to reenter the workforce as an emergency dispatcher. Her husband is back to work as a homebuilder. Eventually, once they’re settled, they’d like another baby, though after Edwards’ hysterectomy, they’ve accepted they will either have to adopt or go through a surrogate. “Indy is the best thing I ever did,” she said, “I’m just so thankful for her and what these doctors did. I’d go through it all over again.”
Resources
- L. Johannesson and A. Enskog, “Experimental uterus transplantation,” Best Pract. Res. Clin. Obstet. Gynaecol., vol. 28, no. 8, pp. 1198–1210, Nov. 2014.
- M. Brännström, “Uterus transplantation and beyond,”
J. Mater. Sci. Mater. Med., vol. 28, no. 5, pp. 1–9, May 2017. - G. Testa et al., “First live birth after uterus transplantation in the United States,” Amer. J. Transplant., vol. 18, no. 5, pp. 1270–1274, May 2018.
- W. Fageeh, H. Raffa, H. Jabbad, and A. Marzouki, “Transplantation of the human uterus,” Int. J. Gynecol. Obstet., vol. 76, no. 3, pp. 245–251, Mar. 2002.
- A. Atala, S. B. Bauer, S. Soker, J. J. Yoo, and A. B. Retik, “Tissue-engineered autologous bladders for patients needing cystoplasty,” Lancet, vol. 367, no. 9518, pp. 1241–1246, Apr. 2006.
- C. Bulletti and C. Simon, “Bioengineered uterus: A path toward ectogenesis,” Fertil. Steril., vol. 112, no. 3, pp. 446–447, Sep. 2019.